
| Home |
| Cough: Options for Self-Treatment W. Steven Pray, Ph.D., R.Ph. US Pharmacist 27(2), 2002. © 2002 Jobson Publishing |
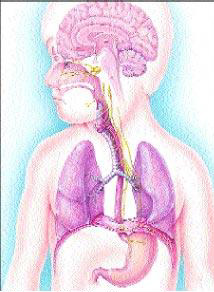
Figure. The cough reflex occurs when certain pulmonary and bronchial receptors in the lungs are irritated.
The Angiotensin Converting Enzyme (ACE) inhibitors have become mainstays in the treatment of hypertension and congestive heart failure since their introduction in the late 1970s.[3] About 2% to 14% of people who are placed on an ACE inhibitor complain of a chronic cough.[4] The onset varies from 3 to 4 weeks to a full year after the initiation of therapy. The cough is typically nonproductive, and worsens at night and whenever the patient assumes a supine position. For these reasons, ACE inhibitor-induced cough is often misdiagnosed as GERD-induced cough. Women and nonsmokers are suffer from ACE inhibitor-induced cough more frequently than other groups. When this type of cough occurs, it is futile to switch to another ACE inhibitor; however, the physician may attempt dose reduction. If this does not help, withdrawal of the medication will effect rapid resolution of cough, and a different group of antihypertensive agents should be chosen.
Cough is a common symptom in patients of virtually all ages. The severity of cough ranges from a mild, barely noticeable, quiet cough to loud, rattling coughs that are accompanied by barking sounds. Many people cough once or twice during the day. These coughs are usually harmless attempts to clear the airways, and need not be treated. However, airway clearance can be facilitated by drinking 8 to 10 eight-ounce glasses of water daily.Cough of the Common Cold
Almost everyone has had a common cold and can recognize its presence. In most cases, it begins with a scratchy or painful throat, followed by nasal congestion and runny nose, and the development of a cough. At first, the cough may help you raise thick secretions in the lungs to prevent pneumonia. These "productive" coughs are beneficial, and should not be stopped. Instead, you should drink lots of water, use a vaporizer or a humidifier, and take a nonprescription product containing guaifenes-in, such as Robitussin.
However, there are times when all other cold symptoms have disappeared, but a cough hangs on for several days. This dry, hacking, nonproductive cough can be halted with the use of such nonprescription ingredients as dextromethorphan (Vicks 44), topical menthol products (Vicks Vaporub, Mentholatum), menthol lozenges or tablets (Hall's), or vaporizer inhalants (Kaz Inhalant, Vicks Inhalant).
If the cough is productive but disrupts sleep, a product containing guaifenesin and dextromethorphan may be the best choice (e.g., Vicks 44-D, Robitussin DM).
When to See a Physician
There are times when a person with cough should have a professional checkup. For instance, cough in those under the age of 2 years should be evaluated by the pediatrician. Any time cough lasts longer than 7 days or recurs, a more serious underlying condition such as cystic fibrosis could be present, and a physician must be seen.
If a cough is not accompanied by runny nose or sore throat, it may not be due to a common cold at all. Some patients already suspect that the cough is caused by another problem. If it is due to smoking, asthma, or is accompanied by excess phlegm, a physician appointment should be made. You may recall a specific event, such as use of a chemical or solvent in a closed place, that preceded the airway irritation. You may have experienced lung damage from the chemical, and a check-up is a wise idea. Certain blood pressure medications ("ACE-inhibitors") can cause a chronic dry cough. If you suspect your cough is a side effect of medication, Consult Your Pharmacist. These vital beneficial medications should not be discontinued without your physician's approval.
You may experience episodes of gastroesophageal reflux, in which stomach contents travel up into the esophagus. As they damage the esophageal tissues, they can also damage some of the airway tissues and produce a cough. You may choose to try several lifestyle modifications, along with such nonprescription products as Gaviscon, Pepcid AC, Zantac 75, Axid AR, or Tagamet HB 200.
Remember, if you have questions, Consult Your Pharmacist.