
| Home |
| News 01/07/2544 |
| Medication Errors The Roles of Pharmacy Educators, Practitioners, and Students in Medication Error Reduction: A Call to Action Sharon Murphy Enright, M.B.A., R.Ph., Murfinc, Richmond, VA; Karen E. Smith, M.S., Pharmacy Practice Consultant, New Berlin, WI; Steven R. Abel, Pharm.D., FASHP, Department of Pharmacy Practice, Purdue University School of Pharmacy and Pharmacal Sciences, Indianapolis, IN; Amanda Clarke, Pharm.D., Drug Information Resident, Purdue University/Eli Lilly and Company, Indianapolis, IN [Medscape Pharmacists, 2001. © 2001 Medscape, Inc.] |
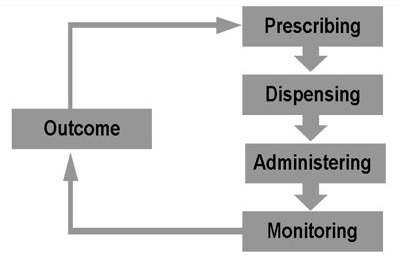
Figure 1.