
| Home |
| News 07/06/2544 |
| TREND OF THE MONTH: EMPLOYERS OFFER DIFFERENT INCENTIVES TO ENCOURAGE GENERIC USE [Drug Benefit Trends 13(4): 11-12, 2001. © 2001 Cliggott Publishing Co., Division of SCP/Cliggott Communications, Inc.] |
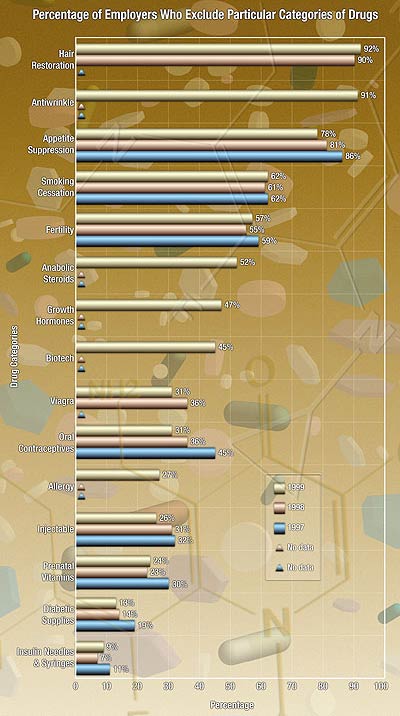
Figure. An employer's decision to exclude a drug or drug category is based on numerous factors, including the cost of the drug to the employer, the availability of a similar therapy in a nonprescription form, the attitude of the employer toward health care benefits, and the competition for hiring and retaining employees.